An AAPM Grand Challenge
 AAPM is sponsoring a challenge for the standardization of imaging and reconstruction protocols of quantitative SPECT/CT acquired after Y-90 microspheres radiotherapy. The results of the challenge will be announced publicly at the Grand Challenge Symposium of the 2022 AAPM Annual Meeting.
AAPM is sponsoring a challenge for the standardization of imaging and reconstruction protocols of quantitative SPECT/CT acquired after Y-90 microspheres radiotherapy. The results of the challenge will be announced publicly at the Grand Challenge Symposium of the 2022 AAPM Annual Meeting.
Limited funding for the materials needed for this challenge will be available on a first come, first serve basis. Participants will receive limited funding contingent on agreeing to submit and make publicly available the image data sets we require for the study. Additionally, one member from each of the two top-performing teams will receive complimentary registration for the 2022 AAPM Annual Meeting.
If seeking funding, please let us know of your participation at the earliest time possible as funding is limited and is first come, first serve. UPDATE (4/4/22): As of this time, we have reached the limit of participants that can be funded. However, since funding is contingent on data submission, we are waitlisting those who still wish to participate and would like support if it becomes available. Please email dianeal@baptisthealth.net to be waitlisted for funding.
- Submission of materials and information from participants:
May 16, 2022
UPDATE (5/12/2022): Due to supplier issues, the deadline for competition has been extended to May 23, 2022. No further extensions are possible. - Winning teams notified of Challenge results:
June 13, 2022
UPDATE (5/12/2022): Due to submission extension, winning teams will be notified no later than June 20, 2022 - Winning results presented at the Grand Challenges Symposium session of the 2022 AAPM Annual Meeting in Washington, D.C.: Monday, July 11th, 2022. (Please note, one member of the winning and runner-up teams will be required to present on their challenge results at this session and will be awarded complimentary Annual Meeting registration in order to attend.)
At the discretion of the Challenge Organizers, submissions may be accepted after the deadline through July 1, 2022. These post-deadline submissions will not be considered eligible for the challenge competition and awards, however, will be accepted for data analysis and inclusion in the forthcoming published challenge report(s).
Participants are encouraged to carry out the Challenge on multiple SPECT/CT scanners if possible (different manufacturer/model/configuration), however, they are limited to one submission as their official entry for the contest. Participant must communicate to organizers which submission they choose to have judged in the challenge. All other entries involving different model scanners will be utilized in the data analysis and inclusion in the forthcoming published challenge report(s) in Medical Physics.
To register as a participant for this Challenge, access the forum, and upload results, please visit the MedICI site.
Once registered, please note that emails with important updates or new posts to the forum may be sent to the spam folder. Please check your spam/junk folder for emails from “MedICI Challenges <kalpathy@mgh.harvard.edu> “. It is highly recommended to whitelist this sender.
SIRPRISE Challenge Format
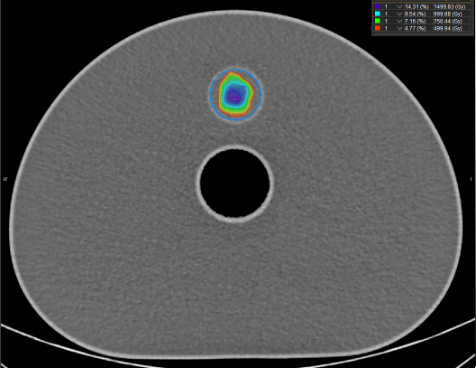
The goal of this challenge is to establish an evidence-based standardized practice of imaging and reconstructing SPECT/CT images of patients who underwent hepatic Y-90 microspheres radiotherapy for the purpose of post-treatment dosimetry. The study aims at imaging a NEMA IEC body phantom with a known quantity of Y-90 chloride using a specified imaging energy window and scattering energy window. After correcting the images for attenuation correction as well as for scatter using a background compensation (BC) technique based on the work of Siman et al. (2016), the images will then be reconstructed as desired and dose maps generated (using specified methods) by the participant. Participants will then submit two completed worksheets, DVH report pdf with specific metrics, and four DICOM image sets: 1. SPECT projections (un-corrected for attenuation, scatter, nor resolution recovery and un-reconstructed); 2. SPECT images reconstructed at the participants discretion after attenuation- and scatter-correction as specified in the challenge instructions; 3. CT scan that is registered to the SPECT study; 4. RT Dose DICOM file of the dose map (using commercial software or in-house software). Participants will upload their information and image data sets to the challenge website.
The challenge organizers will attenuation-and scatter-correct the SPECT projections, reconstruct using the same algorithm for all participants, then calculate dose mapes and generate DVH metrics. The organizers will also calculate dose maps using the participant’s reconstructed SPECT/CT images. These dose maps will be compared to those provided by the participants and analyzed for discrepancies. Additionally, a ground truth will be calculated using a validated phantom-specific Monte Carlo based calculation and compared to the three dose maps: 1. Dose map generated by the participant; 2. Dose map generated by organizers using participant’s reconstructed SPECT images; 3. Dose map generated by organizers using organizer’s reconstructed SPECT images that are based on the participant’s SPECT projection data.
Submissions will be ranked based on how close their computed dose map DVH metrics agree with the ground truth. A winner and runner-up will be chosen based on the DVH metrics that agree best with ground truth. The winner and runner-up (one member per team) will receive complimentary registration to the 2022 AAPM Annual Meeting (July 10-14, 2022).
Scoring information: For the purpose of scoring to declare a winner, the discrepancy between ground truth and each of the four DVH metrics for every volume of interest (VOI) submitted by the participant will be calculated and averaged for each VOI. Then the discrepancy of each VOI will be averaged to arrive to a final discrepancy. See Sections F and G for more information on the VOIs and DVH metrics. Participants will be ranked by their final discrepancy. A lower discrepancy will yield a higher score. The winner will be the participant with the highest score (lowest discrepancy). If the top two participants have the same score, the tie breaker will be D70 of the 37-mm sphere VOI that is closest to ground truth.
Please note, participants may not withdraw from the competition once a submission is made. Multiple submissions may be made but only the latest data will be analyzed and scored for the challenge.
The findings of this Challenge, with participants listed as co-authors, will be published in Medical Physics.
Instructions for Participants
This challenge is utilizing a modified version of the results reported by Siman et al. (2016)1. Please refer to this publication for information on the methodology.
- Site information collection: Please fill out Worksheet A.
- How to setup imaging protocol on your SPECT/CT scanner:
- Primary imaging energy window: 90-125 keV (you may need to enter 107.5 keV as center of EW with +/- 16.3% EW spread or 107.5 keV with 32.6% total EW spread, depending on the configuration of your scanner. Please consult with your manufacturer if unsure).
- Scatter-correcting energy window: 310-410 keV (you may need to enter 360 keV as center of EW with +/- 13.9% EW spread or 360 keV with 27.8% total EW spread, depending on the software configuration of your scanner. Please consult with your manufacturer if unsure).
- Use a medium-energy low-penetration (MELP) collimator.
- Setup SPECT projection image acquisition for 28 s/view for 2x64 views over 360° for each energy window. 128x128 matrix.
- Setup CT acquisition using 120 kVp, 200 mAs. Use 3.75 mm slice thickness, 512x512 matrix, CT resolution: 1 mm x 1 mm x 3.75 mm. Use filtered back projection (FBP) reconstruction.
- Most machines apply corrections on each detected event in real-time, such as uniformity, linearity, energy, isotope decay, and center-of rotation (COR). Allow these corrections to be made as your machine’s manufacturer recommends and specify what corrections are made
- Specifically record and report what was used in the above steps in Worksheet A. Note that if your machine has limitations to these parameters, please set as close to these parameters as possible
- Activity ordering and dose calibrator settings for assay:
- Order 65 mCi of Y-90 chloride (90YCl) in 4 mL from Eckert & Ziegler (they have NIST-traceability). It can be found on this webpage: Yttrium-90 chloride solution - Eckert & Ziegler Radiopharma. It is recommended to order through your radiopharmaceutical pharmacy and to describe its use as research/instrument calibration purposes to ensure best pricing. Order for a calibration date you intend to make your measurements.
- Refer to Worksheet B for complete instructions.
- How to prepare the NEMA IEC Body Phantom for imaging:
- Order the NEMA IEC Body Phantom (if you don’t have one). It can be found on this webpage: https://www.meditest.fr/en/produit/nema-iec-body-phantom-set/ . It is recommended to order through your institution’s preferred supply chain representative for best pricing.
- Follow the manufacturer’s instructions on filling the phantom. Lung insert should be left empty (i.e., filled with air only). Check for water tightness before loading radioactive material.
- Place the largest sphere at the 12 o’clock position. Only the largest sphere (37-mm diameter) and the background compartment will be filled with radioactive material. The remaining five spheres should be left out of the phantom. Practice loading the largest sphere as well as removing air bubbles prior to loading the largest sphere with radioactive material. Effort should be made to minimize air bubbles while avoiding overfilling and causing a spill.
- Refer to Worksheet B for complete instructions.
- How to reconstruct your SPECT images:
- Note: Ensure that your images are not saved over themselves so that the original SPECT projections (i.e., without attenuation or scatter correction) are available after corrections occur as these original images will need to be uploaded as part of the challenge requirements.
- Apply CT-based attenuation correction (AC) to the primary energy window (EW[Primary]) and to the background compensation (EW[BC]) SPECT projections.
- Use the following image math to backscatter compensate (scatter-correct) the primary EW:
EW[Primary, AC+BC corrected] = EW[Primary] – 0.63*EW[BC] (Eqn. 1)
- Participants can choose to reconstruct their images as they see fit after attenuation- and scatter-corrections are made as specified above (using on-board software on SPECT/CT scanner, using 3rd-party commercial software such as MIM, or using in-house software using MLEM, OSEM, etc.) Participant must report which method they chose to reconstruct in Worksheet A.
- Per Siman et al. (2016)1 methodology, it is recommended to use the following parameters for reconstruction:
- Algorithm = OSEM (Ordered Subset Expectation Maximization)
- Equivalent iterations = 128 (subset=8 x iteration=16)
- Matrix size = 128 x 128
- Voxel size = 4.8 mm
- Report the parameters used above in Worksheet A, including standard imaging corrections such as uniformity and decay correction. Participants are allowed to use different parameters for reconstruction and report as such.
- Note, organizers will be reconstructing images based on parameters defined above.
- How to create a dose map:
- Participant may choose to calculate the dose map using commercial software (MIM, Velocity RapidSphere, DosiSoft, Hermes, etc.), or in-house software.
- A total of three VOIs will be needed. Contour the external boundaries of the phantom and the 37-mm sphere. For the sphere, create two VOIs: one with the entire sphere (stem not included), and another one that is 10 mm in diameter located in the center of the sphere (this is to decrease the partial volume effect). Calculate DVH metrics for the two 37-mm sphere VOIs: mean dose, D70, D50, D20.
- Calculate the DVH metrics for the phantom VOI: mean dose, D70, D50, D20. Ensure to subtract out the whole 37-mm sphere contour from the phantom VOI for the DVH metrics.
- Organizers will be using the local deposition model (LDM) with known activity for generation of dose map on MIM Y90-SurePlan software. Organizers will also use phantom-based Monte Carlo methods to create a reference dose map.
- What/how to submit required data for the Challenge:
- Upload the following materials into the MedICI site:
- Worksheets A and B completed (can be typed or handwritten if legible).
- Original SPECT projections (no attenuation- or scatter-correction):
- EW[primary]
- EW[BC]
- AC+BC-corrected SPECT/CT reconstructed images
- EW[primary,AC+BC-corrected] SPECT reconstructed as participant desires
- CT registered to SPECT reconstructed using FBP method (if possible, please send the HU vs. density curve data for your machine)
- Dose map (RTDose file) generated from EW[primary,AC+BC-corrected] SPECT (reconstructed as participant desires) using either commercial or in-house software.
- RTStructure set (and RTPlan, if applicable) DICOM files
- DVH metrics
- VOI: 37 mm sphere
- Mean dose
- D70
- D50
- D20
- VOI: 10 mm within sphere
- Mean dose
- D70
- D50
- D20
- VOI: Phantom VOI (ensure to subtract out the 37 mm sphere from the Phantom VOI)
- Mean dose
- D70
- D50
- D20
- VOI: 37 mm sphere
- Upload the following materials into the MedICI site:
Organizers
- Diane Alvarez, Miami Cancer Institute
- Andy Dezarn, Wake Forest University
- Wendy Siman, University of Colorado
- Peter Kim, Miami Cancer Institute
- Shirin Enger, McGill University
- the AAPM Working Group on Grand Challenges
Contact
For further information, please contact Emily Townley.
Reference:
- Siman W, Mikell JK, Kappadath S. Practical reconstruction protocol for quantitative 90Y bremsstrahlung SPECT/CT. Medical physics. 2016 Sep;43(9):5093-103.