MRI: A Growing Modality In Radiation Therapy
MRI: A Growing Modality In Radiation Therapy
Highlights From Today’s Cutting Edge Medical Physics Research
In recent years, we’ve made great strides in optimizing the integration of MRI in Radiation Oncology. In fact, it’s not difficult to imagine a day when MRI becomes the primary method of therapy planning simulation and image guidance for a variety of treatment indications. While CT has long been the preferred modality for radiation therapy due to its geometric reliability and easy conversion to representation of electron density in support of dose calculations, MRI has been a useful adjunct because of its improved ability to discern soft tissue anatomy.MRI is now recommended for volumetric treatment planning in cervical cancer brachytherapy,1 and CT/MRI fusion is now standard practice in radiation therapy. The application of MRI in radiation oncology is not without its challenges, however. In this inaugural issue of the AAPM Research Spotlight, James Balter offers his perspectives on the growing use of MRI for therapy planning, guidance, and assessment treatment response as well as major areas of research and new opportunities provided by AAPM for its members to improve understanding and utilization of MRI in radiation oncology.
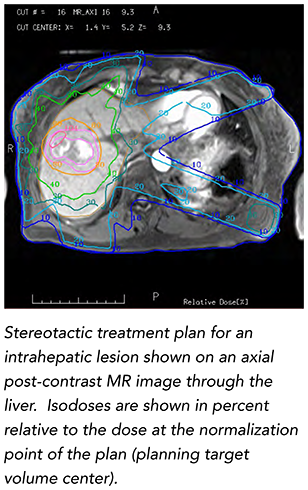 Balter explains that larger magnet bores and improved field homogeneity have supported the potential role of MRI in treatment simulation. Numerous studies indicate that quantitative measurements of perfusion, diffusion, and spectroscopy from MR systems may serve as a biomarker for supporting personalized therapy, supporting assessment of treatment and, if necessary, adaptation mid-therapy course. Various efforts are underway to support MRI in place of CT capabilities by providing a synthetic model of the patient that sufficiently represents radiation attenuation and geometric configuration.2 Vendors are making MRI-compatible immobilization as well as laser-based positioning systems. They are optimizing imaging sequences for the needs of radiation oncology and improving the integration of imaging coils with immobilization systems. Most adaptations to MRI scanners to accommodate radiation therapy simulation primarily require software and inexpensive hardware modifications. As most radiation oncology clinics have access to MRI outside of the department, enhancement of such systems is a cost-effective means of supporting MRI-based simulation for smaller departments.
Balter explains that larger magnet bores and improved field homogeneity have supported the potential role of MRI in treatment simulation. Numerous studies indicate that quantitative measurements of perfusion, diffusion, and spectroscopy from MR systems may serve as a biomarker for supporting personalized therapy, supporting assessment of treatment and, if necessary, adaptation mid-therapy course. Various efforts are underway to support MRI in place of CT capabilities by providing a synthetic model of the patient that sufficiently represents radiation attenuation and geometric configuration.2 Vendors are making MRI-compatible immobilization as well as laser-based positioning systems. They are optimizing imaging sequences for the needs of radiation oncology and improving the integration of imaging coils with immobilization systems. Most adaptations to MRI scanners to accommodate radiation therapy simulation primarily require software and inexpensive hardware modifications. As most radiation oncology clinics have access to MRI outside of the department, enhancement of such systems is a cost-effective means of supporting MRI-based simulation for smaller departments.
Not only is MRI seeing increased use in treatment planning, explained Balter, it is making its way into the treatment room for guidance of therapy delivery. More than a decade ago, Jan Lagendijk and colleagues at the University Medical Center at Utrecht, Netherlands proposed using MRI in conjunction with a linear accelerator for therapy guidance.3 Since then, development of MRI-guided treatment delivery systems (MRgRT) has led to exciting new approaches in treatment that have recently come online or will shortly, including:
- A 0.35 Tesla system with three cobalt treatment heads that supports image-guided positioning, tracking of patient anatomy during treatment and the ability to adapt plans during treatment (ViewRay). This system is being used to treat patients at Washington University, the University of California at Los Angeles, the University of Miami and the University of Wisconsin.
- A linac integrated with a 1.5 Tesla MRI system (Philips, Elekta) under development by Lagendijk and colleagues at Utrecht.3
- A linac integrated with a gantry-mounted 0.2-0.5 Tesla MRI system in a rotating biplanar arrangement developed by Gino Fallone and colleagues at the Cross Cancer Institute in Edmonton.4
- A three-room suite with a mobile high-field MRI scanner, with a brachytherapy unit on one side and a linear accelerator on the other, providing the ability to perform scans of the patient on the treatment couch, which then can be turned around and used for patient treatment, under development by David Jaffray and colleagues at the Princess Margaret Cancer Centre, Toronto, Ontario.5
"Further integration of MRI in Radiation Oncology will require changes to education and practice," says Balter. "Magnetic field safety and interference with other imaging and treatment systems need to be considered in design and installation of MRI in Radiation Oncology departments." Along these lines, MRI-specific quality assurance5, as well as modified treatment QA for systems integrated with MRI are areas that need to be considered, presenting an important area of research by AAPM physicists. Balter went on to explain that the quantitative use of MRI requires special vigilance regarding imaging scan parameters and analysis methods, as well as development of additional measurements to ensure that the different needs of Radiation Oncology versus diagnostic radiology are met.6
"As with any significant medical advance, there are concomitant demands and challenges," explains Balter, "and foremost is the need to educate medical physicists." To that end, AAPM is offering a new Certificate Course at its Annual Meeting dedicated to the topic of MRI in Radiation Therapy. The Certificate Course will be held Wednesday, July 15, at the AAPM’s 57th Annual Meeting & Exhibition in Anaheim and will include five sessions: two educational sessions, two symposia, and one proffered paper session. The symposia and sessions are open to all meeting registrants, with the certificate component (including online evaluations, etc.) available via additional registration. For more information, visit the Annual Meeting website.
- Dimopoulos J, Petrow P, Tanderup K, et al. Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group (IV): basic principles and parameters for MR imaging within the frame of image based adaptive cervix cancer brachytherapy. Radiother oncol. 2012;103(1):113-22.
- Hsu S, Cao Y, Huang K, Feng M and Balter J. Investigation of a method for generating synthetic CT models from MRI scans of the head and neck for radiation therapy. Phys Med Biol. 2013;(58): 8419-35.
- Lagendijk J, Raaymakers B and van Vulpen M. The magnetic resonance imaging-linac system. Semin Radiat Oncol. 2014 Jul;24(3): 207-9.
- Fallone BG, Murray B, Rathee S, et al. First MR images obtained during megavoltage photon irradiation from a prototype integrated linac-MR system. Med Phys 2014; 36(6): 2084-2088.
- Jaffray D, Carlone M, Milosevic M, et al. A facility for magnetic resonance-guided radiation therapy. Semin Radiat Oncol. 2014;24(3):193-5.
- Paulson E, Erickson B, Schultz C and Li X. Comprehensive MRI simulation methodology using a dedicated MRI scanner in radiation oncology for external beam radiation treatment planning. Med Phys. 2015;42(1):28-39.